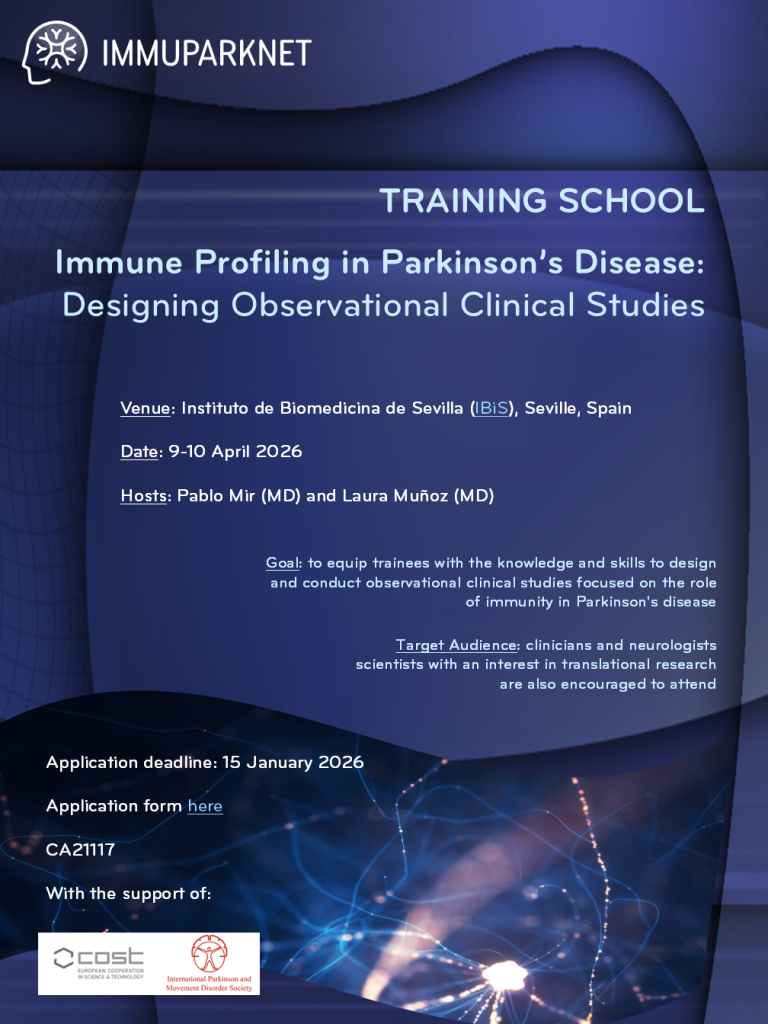
We are pleased to invite you to the upcoming IMMUPARKNET Training School on Immune Profiling in Parkinson’s Disease: Designing Observational Clinical Studies
Venue: Instituto de Biomedicina de Sevilla (IBiS), Seville, Spain
Date: 9-10 April 2026
Hosts: Pablo Mir (MD) and Laura Muñoz (MD)
Goal: to equip trainees with the knowledge and skills to design and conduct observational clinical studies focused on the role of immunity in Parkinson’s disease
Target Audience: clinicians and neurologists; scientists with an interest in translational research are also encouraged to attend
Application deadline: 15 January 2026
Available spots: 16-20 students
Application criteria: CV and motiantion
** All selected students will have their long distance travel and per diem reimbursement supported by COST **
Submit your application here
This training school aims to equip neurologists with the knowledge and skills to design and conduct observational clinical studies focused on the role of immunity in Parkinson’s disease. This course is primarily designed for clinicians and neurologists but basic scientists with an interest in translational research are also encouraged to attend, fostering interdisciplinary collaboration between clinical and research communities in the line with IMMUPARKNET. The training school will cover the following key topics to guide neurologists in designing robust observational clinical studies on immunity in Parkinson’s disease: Criteria for inclusion and exclusion of participants, study design, clinical data and patient stratification, brain imaging and biomarkers of neuroinflammation, biological samples and immune biomarkers.
TRAINING SCHOOL – PRELIMINARY AGENDA
DAY 1 – THURSDAY 9th April
8.30h Registration Opens
9.00h Welcome and Action Presentation by Action Chair, Prof. Cristoforo Comi and Training School Director, Pablo Mir.
9.15 – 10.00 h – Session 1. Parkinson’s Disease and the Immune System: Unraveling Their Interplay – Speaker: to be confirmed.
Content: The session opens with a concise introduction to Parkinson’s disease, covering key clinical features and core pathophysiological hallmarks. This is followed by a brief primer on immune system fundamentals and the gut–brain axis. This presentation then will present a summary of the central and peripheral immune mechanisms described in PD, highlighting major inconsistencies in human data and discusses limitations in current observational research.
Learning Outcomes: Participants will acquire basic knowledge about the immune system, as well as the clinical picture of Parkinson’s disease. Finally, participants will recognize the potential role of immune dysregulation in PD and the critical need for well-designed, standardized protocols in immunological studies of PD.
10.05 – 10.45 h Session 2. Who should be included in observational studies of immunity in Parkinson’s Disease? – Speaker: Caroline Williams-Gray
Content: to discuss inclusion and exclusion criteria of the participants, including the two-step approach for core/extended studies. Age/sex matching. Handling comorbidities like diabetes or vaccinations. Emphasis on minimizing confounders for PD-specific immune signatures. –
10.45-11.15. Q/A + Participant flash work presentation related to Session 2.
11.15h – 11.45 Coffee Break
11.50 – 12.30 – Session 3. Cross-sectional or longitudinal: which design best addresses immune hypotheses in Parkinson’s disease? – Speaker: Cristoforo Comi
Content: covering the pros/cons of each (e.g., hypothesis generation in cross-sectional vs. causality in longitudinal), and challenges like patient retention and costs.
12.30 – 13.00 – Q/A + Participant flash work presentation related to Session 3.
13.00 – 15h Lunch break
15.00h – 15.40 h Session 4. How can clinical phenotyping and stratification reveal immune subtypes in Parkinson’s disease? – Speaker: Pablo Mir
Content: Stratification by age/sex, genetics (e.g., LRRK2, GBA), LEDD, motor scales (HY, MDS-UPDRS), cognitive tools (MoCA, PD-CRS), and non-motor assessments (NMSS, GIDS-PD, UPSIT). Explanation should link with immune profiles (e.g., proinflammatory states in severe phenotypes).
15.40-16.10 Q/A + Participant flash work presentation related to Session 4.
16.10 – 18h. Practical Activity 1. Spotlight on your research: Participant presentations and collaborative methodological refinement.
Participants will briefly present their current research/study designs (5-7 min each). After each presentation, the group will brainstorm concrete improvements, focusing on strengthening methodology.
18.00 – 18.30 Guided Tour of Research and Clinical Facilities at Institute of Biomedicine (IBiS) and Hospital Universitario Virgen del Rocío – by Pablo Mir and Laura Muñoz
20h. Dinner
DAY 2 – FRIDAY 10th April
9.00 -9.40 h. Session 5. Can PET imaging detect and quantify neuroinflammation in Parkinson’s disease?
Content: PET imaging (e.g., TSPO radioligands like [11C]PK11195), limitations (e.g., rs6971 polymorphism), and its role in quantifying central neuroinflammation. – Speaker: Edoardo do Natale
9.40 – 10.10 Q/A + Participant flash work presentation related to Session 5.
10.10– 10.40 h Session 6. How can MRI be useful to assess neuroinflammatory processes in Parkinson’s disease? – Speaker: Gaetan Garraux
Content. MRI as complementary to PET; iron-sensitive sequences; microglial activation markers; atrophy & connectivity. Interpret multimodal imaging data (MRI+PET+clinical).
10.40-11.10 Q/A + Participant flash work presentation related to Session 6.
11.10 h-11.40 Coffee break
11.40-12.20 h Session 7: How do we ensure optimal blood collection and preservation of PBMCs for immune profiling in PD?– Speaker: Diego Clemente
Content: Best practices for peripheral blood sampling (particularly PBMCs and PMNCs, but also cytokines)-including circadian cycles-, processing (e.g., timing, temperature), and long-term storage; impact on immune cell subsets and cytokines. Focused on blood, but mention also CSF please.
12.20 – 12.50 h Q/A + Participant flash work presentation related to Session 7.
13.00h – 15 h Lunch
15.00 – 15.40 h – Session 8. Beyond blood, what can faecal samples reveal about gut immunity in Parkinson’s disease? – Speaker: Marta Camacho
Content: sample obtention and handling of faeces. Session particularly focused on faecal samples and the study of gastrointestinal inflammation and immune responses in the gut. –
15.40 – 16.10 Q/A + Participant flash work presentation related to Session 8.
16.10-17.40 Practical Activity 2 – Design your own immunity study in Parkinson’s disease.
Participants will be asked to work in small groups to design a study to address a specific question around immunity in PD – putting into practice what they have learnt in this two-day course. Each small group will deliver a concise 5-minute presentation to the full group, followed by 2–3 minutes of peer Q&A
17.40h End of the Training School by Cristoforo and Pablo.
___________________
Training School with the support from COST Action CA21117